Hip Replacement Surgery
Rocky Mount, NC


Where is Your Pain?
Request Appointment
ARE YOU SUFFERING FROM CHRONIC HIP PAIN THAT LIMITS YOUR MOBILITY?
Hip pain can transform simple daily tasks into painful challenges that diminish your independence and quality of life. When the ball-and-socket joint connecting your thighbone to your pelvis becomes damaged through arthritis, injury, or disease, every step can trigger sharp, grinding discomfort that radiates through your groin and thigh. While hip problems often develop gradually in older adults as cartilage wears away, debilitating hip conditions can strike at any age.
Degenerative diseases, autoimmune disorders, traumatic injuries, and bone tissue death can all devastate your hip joint, creating persistent pain that steals your ability to walk comfortably, climb stairs, or simply bend down to tie your shoes. You don’t have to accept a sedentary lifestyle dictated by hip dysfunction. Carolina Regional Orthopaedics offers both surgical and conservative hip treatment options precisely matched to your condition.
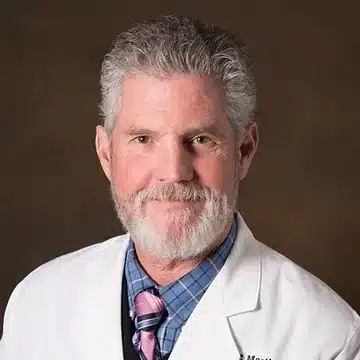
Our hip replacement specialists at Carolina Regional Orthopaedics, led by Dr. Bernard P. Kemker, Director of Joint Replacement Services, understand the profound impact hip pain creates in your daily life. We have helped countless Rocky Mount, NC, patients reclaim pain-free movement through personalized treatment approaches that prioritize your long-term success.
Contact us if chronic hip pain has begun controlling your life or if you suspect hip replacement might offer the relief other treatments haven’t delivered. Our joint replacement team begins with comprehensive evaluation and conservative care, recommending surgery only when your hip damage has progressed beyond what non-operative treatments can address.
WHAT IS HIP REPLACEMENT SURGERY?
Hip replacement surgery directly addresses this mechanical breakdown by removing the damaged portions of your hip joint and installing precision-engineered prosthetic components that restore smooth, pain-free movement. This procedure, medically termed total hip arthroplasty, stands among the most successful operations performed in modern medicine, with over 450,000 Americans undergoing the surgery annually and success rates consistently exceeding 95%.
Surgeons recommend hip replacement when your damaged joint no longer responds to conservative interventions—when physical therapy, weight management, medications, and targeted injections fail to provide meaningful relief. The decision hinges on whether hip pain prevents you from maintaining your desired lifestyle, disrupts your sleep, or forces you to abandon activities that once brought joy.
The replacement procedure removes both your worn femoral head and damaged acetabular socket, securing new artificial components to the healthy bone that remains. Modern prosthetic hips typically combine a metal or ceramic ball, a metal socket, and an ultra-smooth plastic or ceramic liner that allows effortless gliding motion. These sophisticated implants are engineered from biocompatible materials designed to withstand decades of use—more than half of all hip replacements now last 25 years or longer.
Carolina Regional Orthopaedics performs hip replacement using both anterior (front) and posterior (back) surgical approaches, allowing Dr. Kemker and our surgical team to select the technique best suited to your specific anatomy, body type, and medical needs. This surgical flexibility ensures you receive truly personalized care rather than a one-size-fits-all approach.
WHAT ARE THE COMMON CONDITIONS THAT REQUIRE HIP REPLACEMENT?
Hip replacement becomes necessary when the joint sustains damage severe enough that conservative treatments can no longer maintain acceptable function or comfort. Several distinct conditions drive patients toward surgical reconstruction, each attacking the hip through different mechanisms but ultimately producing similar devastating results.
Osteoarthritis dominates as the leading cause of hip replacement in America, responsible for the vast majority of procedures. This wear-and-tear arthritis develops as decades of use gradually erode the slippery cartilage caps protecting your bones. Picture tire tread wearing down to expose the underlying rubber, as hip cartilage thins and roughens, your bones begin grinding directly against each other with every movement. The result manifests as deep, aching pain centered in your groin, progressive stiffness that makes mornings miserable, and steadily worsening difficulty with activities like walking, climbing stairs, or getting out of low chairs.
Rheumatoid arthritis takes a fundamentally different destructive path. This autoimmune disorder causes your immune system to mistakenly attack the synovial lining of your joints, triggering waves of inflammation that eat away at cartilage and bone. Unlike osteoarthritis’s gradual progression, rheumatoid arthritis can rapidly devastate previously healthy hips, leaving joints swollen, tender, and progressively deformed. When medications fail to control the disease’s assault on your hip joint, replacement surgery offers the only reliable path to restored function.
Avascular necrosis, also called osteonecrosis, occurs when blood supply to the femoral head becomes disrupted, starving bone tissue of oxygen and nutrients. Without adequate blood flow, sections of your femoral head literally die and begin to collapse. Trauma from hip fractures or dislocations can sever blood vessels, while prolonged corticosteroid use and excessive alcohol consumption damage the tiny vessels feeding your hip. As dead bone crumbles under your body weight, the hip joint deteriorates rapidly, often requiring replacement to restore stability and eliminate the intense pain that characterizes advanced osteonecrosis.
Hip fractures themselves frequently necessitate replacement surgery, particularly fractures involving the femoral neck—the narrow section of bone connecting the ball to the main thighbone shaft. These injuries plague older adults with osteoporosis, whose brittle bones can fracture from simple falls or even normal walking. When fractures shatter the femoral head or disrupt blood supply, replacement often proves more reliable than attempting to repair the damaged bone, allowing patients to regain mobility quickly rather than spending months immobilized while fractures heal.
Benefits of Hip Replacement Surgery
Freedom from relentless pain: Imagine waking without that familiar deep ache throbbing through your groin. Picture climbing stairs without wincing, sleeping through the night undisturbed by sharp twinges when you shift position. Over 95% of hip replacement patients experience dramatic pain relief—the bone-on-bone grinding that characterized severe arthritis simply disappears once prosthetic components restore smooth gliding surfaces.
Movement reclaimed: Remember bending down to tie your shoes without strategizing the least painful angle? The simple act of getting into your car without careful maneuvering? Hip replacement rebuilds your mechanical advantage, restoring ranges of motion that arthritis had progressively stolen. Patients regain the ability to walk without limping, navigate stairs comfortably, and perform daily tasks that had become agonizing ordeals.
Independence restored: The dignity of bathing yourself, dressing without assistance, preparing your own meals—these basic activities of daily living return after successful hip replacement. The procedure eliminates the physical barriers that had made you dependent on others for simple tasks, returning the self-sufficiency most people take for granted.
Decades of durability: Modern hip implants benefit from engineering refinements spanning half a century. Today’s prosthetic joints routinely function for 20-30 years, with many patients never requiring revision surgery in their lifetime. The materials resisting wear, the designs promoting bone integration, the surgical techniques ensuring proper alignment—every aspect has evolved to maximize longevity.
Faster recovery than you’d expect: Anterior approach patients often walk the same day as surgery. Many discontinue walkers within weeks rather than months. Advanced pain management protocols, minimally invasive techniques, and enhanced recovery programs mean you’ll likely return to modified activities far sooner than hip replacement patients of previous generations.
MOST COMMON HIP REPLACEMENT PROCEDURES AT CRO
Your hip endures tremendous mechanical stress, forces exceeding three times your body weight compress the joint with every step you take. Climbing stairs multiplies that load even further. When decades of this repetitive stress destroy your hip’s protective cartilage, or when injury compromises the joint’s structural integrity, our Rocky Mount surgical team offers proven solutions to restore pain-free mobility.
TOTAL HIP REPLACEMENT
Total hip replacement addresses severe damage affecting both the ball (femoral head) and socket (acetabulum). This comprehensive approach removes diseased bone and cartilage, replacing them with prosthetic components engineered to replicate your natural hip’s smooth motion.
Dr. Kemker and our surgical team remove the damaged femoral head and prepare the thighbone to accommodate a metal stem, typically titanium or cobalt-chromium. This stem anchors inside your femur, either secured with bone cement or designed for cementless fixation where bone grows into the metal surface. A metal or ceramic ball attaches to the stem, forming the new femoral head.
Your damaged acetabulum receives a metal cup pressed into your pelvic bone. Inside this cup sits a specialized liner, most commonly ultra-high molecular weight polyethylene, though ceramic liners offer alternatives. This smooth liner provides the gliding surface where your new ball rotates.
We recommend total hip replacement when arthritis has degraded your entire joint, leaving no viable cartilage. Patients with severe osteoarthritis, advanced rheumatoid arthritis, or extensive post-traumatic damage typically require this reconstruction. Modern implants last 20-25+ years in the majority of patients.
Your hospital stay typically spans one to three days. Physical therapy begins within hours, you’ll take your first assisted steps the same day or morning after surgery. Most patients transition from walker to cane within 3-6 weeks, with complete functional recovery requiring 3-6 months of progressive rehabilitation.
PARTIAL HIP REPLACEMENT
Partial hip replacement—hemiarthroplasty—targets only the femoral head while preserving your natural acetabulum. This streamlined approach suits specific scenarios where the socket remains relatively healthy despite severe damage to the ball.
Surgeons remove the damaged femoral head, prepare the thighbone’s canal, and insert a metal stem with attached prosthetic ball. Rather than resurfacing your acetabulum, this new ball articulates directly against your natural socket cartilage.
We typically reserve partial hip replacement for elderly patients who sustain femoral neck fractures when their acetabular cartilage remains in good condition. This approach makes particular sense for less active individuals whose natural socket can withstand the demands of the prosthetic femoral head. The surgery requires less operative time than total hip replacement and involves less extensive bone removal.
Recovery from partial hip replacement follows a similar timeline to total hip replacement, with patients beginning assisted walking within a day of surgery. Rehabilitation emphasizes restoring hip strength and range of motion through progressively challenging exercises.
Your orthopedic surgeon determines which procedure—total or partial—best addresses your condition based on evaluation of your hip damage pattern, activity level, overall health, and treatment goals.
WHEN IS HIP REPLACEMENT SURGERY NECESSARY?
Hip replacement becomes the recommended intervention when conservative treatments have exhausted their potential and your hip damage requires surgical reconstruction.
Chronic, debilitating hip pain that persists despite comprehensive conservative treatment represents the primary indicator. If months of physical therapy, weight management, anti-inflammatory medications, activity modifications, and corticosteroid injections have failed to provide meaningful relief, your hip damage has likely progressed beyond non-operative approaches. Pain that wakes you at night or prevents you from walking more than a few blocks demands more definitive intervention.
Severe mobility limitations that compromise your independence justify surgical consideration. When hip stiffness prevents you from tying your shoes, when pain makes climbing stairs an ordeal, when getting in and out of your car demands careful choreography—these functional losses indicate your hip joint can no longer support your basic needs.
Radiographic evidence of advanced joint destruction provides objective confirmation. X-rays revealing complete cartilage loss, bone-on-bone contact, acetabular wear, or femoral head deformity confirm the mechanical breakdown causing your symptoms. When imaging demonstrates severe structural damage, conservative treatments address only symptoms rather than the underlying problem.
The decision ultimately rests on one fundamental question: Does your hip pain and dysfunction prevent you from living the life you deserve? When you find yourself declining social invitations because walking is too painful, when you’ve stopped activities you once loved—that’s when hip replacement transitions from future consideration to current solution.
AGE AND CANDIDACY CONSIDERATIONS
Age alone doesn’t disqualify you from hip replacement, the procedure spans patients from their 40s through their 90s. What matters is whether your overall health can withstand major surgery and whether your hip damage justifies the intervention regardless of your birth year.
Younger patients—those under 60—face unique considerations. Higher activity levels and longer life expectancy mean increased cumulative stress on prosthetic components, potentially necessitating revision surgery decades down the road. However, modern implants demonstrate impressive durability even in active younger patients, with recent data showing 10-year survivorship rates exceeding 94% in patients under 55. Living with severe hip pain through your 40s and 50s while waiting for some arbitrary age threshold makes little sense when replacement can restore decades of pain-free function.
Older patients—those over 75—sometimes worry they’re “too old” for hip replacement. Yet advanced age itself poses minimal barriers when overall health remains good. In fact, hip fracture patients in their 80s and 90s routinely undergo replacement to avoid the devastating complications of prolonged immobility. The surgery’s ability to quickly restore mobility often proves lifesaving in elderly patients who would otherwise become bedridden.
MEDICAL HEALTH FACTORS
Your candidacy depends more heavily on managing chronic conditions than on age or activity level. Uncontrolled diabetes dramatically increases infection risk and impairs wound healing—achieving good blood sugar control before surgery proves essential. Significant heart disease requires cardiac clearance and careful anesthetic planning. Active infections anywhere in your body must resolve completely before hip replacement, as bacteria could seed your new prosthetic joint.
Severe obesity, typically defined as BMI over 40, substantially elevates surgical risks including wound complications, infections, and implant failure. Many surgeons require weight loss before proceeding with elective hip replacement, both to reduce operative risks and improve long-term outcomes. Even modest weight reduction significantly decreases stress on your new hip while lowering complication rates.
ORTHOPEDIC CONDITIONS FREQUENTLY TREATED WITH HIP REPLACEMENT
OSTEOARTHRITIS
Cartilage breakdown defines osteoarthritis. What begins as occasional stiffness progresses toward constant pain and severe mobility restriction. Early-stage osteoarthritis responds to conservative management: physical therapy, weight loss, anti-inflammatory medications, and injections.
But osteoarthritis inevitably worsens. As cartilage continues thinning, pain transitions from activity-related to constant. Your hip stiffens, bone spurs develop, and eventually cartilage erodes completely, leaving bone grinding on bone—a mechanical problem medication cannot fix.
Hip replacement becomes necessary when cartilage destruction crosses this threshold, when conservative treatments no longer provide acceptable relief, when pain prevents sleep or basic activities.
RHEUMATOID ARTHRITIS
Autoimmune destruction creates different urgency. Rheumatoid arthritis attacks joint linings with inflammatory cells that erode cartilage and bone simultaneously. Unlike osteoarthritis’s gradual progression, rheumatoid arthritis can devastate hips within years.
Disease-modifying medications attempt to slow the assault, but many patients still develop severe hip damage requiring replacement. Surgery eliminates the destroyed joint, removing a major source of pain and often allowing reduction in systemic medications.
AVASCULAR NECROSIS
Blood supply disruption starves your femoral head of oxygen, causing bone tissue to die and collapse. The condition develops through hip fractures, prolonged corticosteroid use, excessive alcohol consumption, or sometimes no identifiable cause.
Early-stage avascular necrosis sometimes responds to core decompression, but once significant bone collapse occurs, only hip replacement reliably restores function. The dead, crumbling bone cannot support your body weight.
HIP FRACTURES
Broken hips in elderly patients often demand replacement rather than repair. Femoral neck fractures frequently disrupt blood supply to the femoral head. Attempting repair with pins or screws risks the femoral head dying from lack of blood flow.
Partial hip replacement typically suffices for isolated femoral neck fractures when the acetabulum remains healthy. However, pre-existing acetabular arthritis may warrant total hip replacement to address both the fracture and underlying joint disease.
IS IT TIME TO GET HELP WITH YOUR HIP PAIN?
Persistent hip pain doesn’t represent normal aging. Our board-certified hip replacement specialists diagnose your joint damage through clinical examination and advanced imaging, then develop treatment plans—surgical or conservative—matched to your condition and personal goals.
We utilize cutting-edge surgical techniques including both anterior and posterior approaches, modern implant technology proven to last decades, and comprehensive rehabilitation programs. Our mission focuses on restoring your mobility and eliminating the hip pain that has limited your life.
Ready to schedule your hip replacement evaluation? Call (252) 443-0400 today or use our online appointment form to meet with Dr. Kemker and our joint replacement team at our Rocky Mount location.
Request an Appointment Online
Carolina Regional Orthopaedics, PA allows you to easily schedule an appointment online 24 hours a day, so you can continue your day with little disruption.
Our Providers
At Carolina Regional Orthopaedics, PA, all of our providers are Board Certified Orthopedic Surgeons or

Bernard P. Kemker, MD

Glenn E. MacNichol, MD
Robert C. Martin, DO

Mark N. Perlmutter, MS, MD

Morgan M. Batchelor, PA-C

VanTreia M. Gross, PA-C

Paul Kelley, PA-C

William J. Mayo, PA-C
Our Locations
Orthopedics Rocky Mount
Carolina Regional Orthopaedics, PA
Mon-Thurs
Address:
110 Patrick Ct, Rocky Mount, NC 27804
Hours:
Monday- Thursday: 8 AM - 6 PM
Closed
Friday - Sunday
Phone: 252-443-0400
Fax: 252-443-0572
Pain Management Clinic Tarboro
Carolina Regional Orthopaedics, PA
Tuesdays Only
Address:
101 Clinic Dr. Ste. 7A, Tarboro, NC 27886
Hours:
Tuesday: 8 AM - 5 PM
Closed:
Sunday - Monday, Wednesday - Saturday
Phone: 252-443-0400
Fax: 252-443-0572